
Long before high-speed internet networks made it fast and easy to transfer information, access services, and communicate with others the world over, VA had experimented with ways to deliver health care at a distance. One of VA’s first forays into telehealth occurred in 1959 when the Nebraska Psychiatric Institute set up a two-way television system to conduct group therapy sessions with Veterans at the Omaha VA Medical Center and other VA sites in the state.
A few years later, VA physicians in Boston teamed up with Massachusetts General Hospital (MGH) and the New England Telephone Company on a telehealth project that allowed for remote monitoring of a patient’s vitals. Sensors by the patient’s bed or wheelchair picked up electrical signals from electrodes attached to the body and transmitted them via telephone lines to a device in the doctor’s office that functioned like a cardiogram.
In the early 1970s, Veterans at the VA Hospital in Bedford, Massachusetts, were the beneficiaries of another early telehealth venture involving Massachusetts General Hospital. In 1968, MGH set up a telehealth medical station staffed by nurses at Boston’s Logan International Airport, employing an interactive video system to connect travelers and airport employees with doctors at the hospital. MGH then expanded its telehealth network to include patients at the VA facility.
The technology was still in its infancy and relied on a microwave relay to transmit video, audio, and physiological data collected from examinations. Even within the limits of the system, however, VA patients were able to receive medical care in specialties ranging from psychiatry and radiology to internal diseases and dermatology.
While these early initiatives were promising, they occurred in isolation and often petered out over time. For instance, Massachusetts General Hospital ended its telehealth program in the mid-1980s. However, the advent of internet-based telecommunications technology in the 1990s revived interest in telehealth across the VA medical system. From 1994 to 2003, thirty different VA medical centers launched pilot telehealth programs and research studies in select fields of medicine. These efforts were localized in nature, usually grant funded, and came about through clinical staff acting on their own initiative.
The virtual dermatology clinic created at the John J. Pershing VA Medical Center in Poplar Bluff, Missouri, in 1997 was typical of the start-up telehealth programs of the time. It began with a conversation between Timothy S. Moore, the center’s first telehealth coordinator, and his supervisor, who had just purchased a cart full of telecommunications gear and wanted to know if Moore had any thoughts on how to use it. He called around to other hospitals in the Heartland VA Network (the geographical region centered on Missouri and Kansas) and connected with the chief dermatologist at the Harry S. Truman Memorial Veterans’ Hospital in Columbia.
At the doctor’s request, he set up a teledermatology clinic at the Poplar Bluff facility. A nurse practitioner conducted the exam while he operated the equipment. Digital images of potentially pathological areas of the skin taken during the exam were then transmitted to Columbia for subsequent evaluation by dermatology specialists. This form of telehealth, known as Store & Forward, is asynchronous since the remote physician is not interacting with the patient in real-time.

The positive outcomes reported by Poplar Bluff and other telehealth programs coupled with continued investment in VA’s IT infrastructure and videoconferencing capabilities led to the rapid expansion of the agency’s telehealth activities after 2004. By 2010, VA was managing national telehealth programs that provided care to Veterans in 44 different clinical areas.
These programs have proved particularly important to meeting the health care needs of Veterans residing in rural areas, who comprise roughly 33 percent of the nation’s Veteran population. Many of these veterans experience geographic barriers to accessing in-person VA care and would have otherwise needed to travel long distances to reach their nearest hospital or clinic. In-home telemonitoring services have also been a great boon to Veterans with chronic health conditions, leading to fewer trips to the clinic and reducing the risk of hospitalization or complications..
Even before the COVID-19 virus hit the United States in March 2020, VA had established itself as the nation’s largest provider of telehealth care. In 2017, the agency rolled out VA Video Connect, an app enabling Veterans with a computer, tablet, or smart phone connected to the Internet to consult VA providers over live video. VA Video Connect and other technologies helped VA meet the soaring demand for telehealth services during the pandemic. In fiscal year 2021, over 2.3 million Veterans used some form of VA telehealth, a figure that represented about one-third of all Veterans receiving care from VA during this time period. Once a novelty, telehealth has become a core component of VA’s medical system.
The telehealth cart first used at the Poplar Bluff VA hospital in the late 1990s remained in the Heartland Network’s inventory until 2022, when it was accessioned into the permanent collection of the National VA History Center in Dayton, Ohio. Now a historic artifact, the cart attests to VA’s early commitment to finding innovative ways to improve Veteran access to health care.

By Katie Rories, Historian, Veterans Health Administration
Share this story
Related Stories
History of VA in 100 Objects
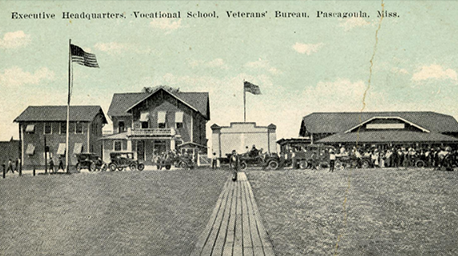
Object 96: Postcard of Veterans Vocational School
In 1918, the government created the first nationwide vocational training system to help disabled Veterans acquire new occupational skills and find meaningful work. Over the next 10 years, more than 100,000 Veterans completed training programs in every field from agriculture and manufacturing to business and photography.
History of VA in 100 Objects
Object 95: 1840 Census of Pensioners
In a first, the 1840 census collected data on Veterans and widows receiving a pension from the federal government. The government published its findings in a stand-alone volume titled “A Census of Pensioners for Revolutionary or Military Services.”

History of VA in 100 Objects
Object 94: Southern Branch of the National Home
The Southern Branch of the National Home for Disabled Volunteer Soldiers opened in Hampton, Virginia, in late 1870. The circumstances surrounding the purchase of the property, however, prompted an investigation into the first president of the National Home’s Board of Managers, Benjamin Butler.


