
After the Civil War, the Central Branch of the National Home for Disabled Volunteer Soldiers in Dayton, Ohio, and the Southern Branch in Hampton, Virginia, opened their doors to Union Veterans without regard to skin color. The men admitted to these branches found themselves living in two of the nation’s first racially integrated federal institutions.
By the turn of the century, however, the landmark Supreme Court ruling Plessy v. Ferguson allowed institutionalized racism and segregation to prevail in American society. Many Veterans hospitals followed the policies adopted by the military and medical communities and made racial segregation the rule.
To accommodate the growing number of African American Veterans in the south following World War I, the Veterans Bureau opened a hospital in Tuskegee, Alabama, in 1923 reserved exclusively for their use. Originally called the “Hospital for Sick and Injured Colored World War Veterans,” the installation was staffed entirely by Black doctors and nurses.
Joseph H. Ward, a prominent Indiana physician who served in the U.S. Army Medical Corps during World War I and afterwards rose to the rank of lieutenant colonel, became the hospital’s director. He was the first African American to hold this position in VA history. The Tuskegee facility operated as the VA’s only Black Veterans’ hospital for thirty-one years, providing care for more than 300,000 former servicemembers.
Throughout the 1920s and 1930s, the VA allowed hospitals to choose their segregation status based on local and regional practices. As a result, many VA hospitals, primarily in the south, maintained separate wards for White and Black Veterans. If a hospital did not have segregated facilities, Black patients would only be admitted in emergency cases until they could be transferred to hospitals that did treat African Americans.
At the end of World War II, knowing that more than a million Black servicemembers would soon be returning to civilian life, the VA explored building another hospital for African American Veterans in Mississippi. However, the National Association for the Advancement of Colored People (NAACP) argued against establishing more racially segregated hospitals like Tuskegee. The NAACP urged VA to fully integrate all hospitals, arguing that “There is no reason whatever why colored and white Veterans should be treated in separate hospitals after having fought and bled together to make victory possible.”
President Harry S. Truman signed Executive Order 9981 desegregating the U.S. Armed Forces in July 1948. While the order applied to VA medical installations in theory, forty-seven of the 166 VA hospitals remained segregated in some form through 1953. That same year, VA Administrator Harvey V. Higley assured NAACP officials that he supported their goals: “We find any semblance of segregation unsocial, uneconomical, and undesirable and we hope the day is not far removed when there will be no semblance of racial segregation in VA Hospitals.”
True to his word, he directed VA facilities that still sanctioned some form of racial segregation to end the practice as quickly as possible. On July 28, 1954, the agency formally announced that segregation had been eliminated at all VA hospitals.
By Katie Rories
Historian, Veterans Health Administration
Share this story
Related Stories
History of VA in 100 Objects
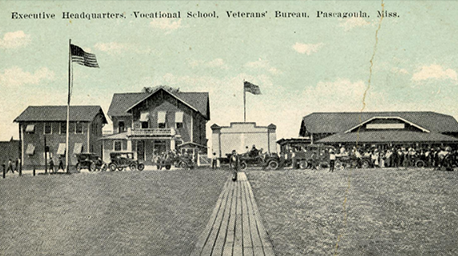
Object 96: Postcard of Veterans Vocational School
In 1918, the government created the first nationwide vocational training system to help disabled Veterans acquire new occupational skills and find meaningful work. Over the next 10 years, more than 100,000 Veterans completed training programs in every field from agriculture and manufacturing to business and photography.
History of VA in 100 Objects
Object 95: 1840 Census of Pensioners
In a first, the 1840 census collected data on Veterans and widows receiving a pension from the federal government. The government published its findings in a stand-alone volume titled “A Census of Pensioners for Revolutionary or Military Services.”

History of VA in 100 Objects
Object 94: Southern Branch of the National Home
The Southern Branch of the National Home for Disabled Volunteer Soldiers opened in Hampton, Virginia, in late 1870. The circumstances surrounding the purchase of the property, however, prompted an investigation into the first president of the National Home’s Board of Managers, Benjamin Butler.



