The federal government first began offering medical care to military Veterans in an institutional setting in the early 19th century. The U.S. Naval Asylum in Philadelphia opened in 1834, followed by the U.S. Soldiers’ Home in Washington, D.C., in 1851. Initially, only careerists with 20 or more years of service in the Navy or Regular Army were eligible for admission to these facilities. After the Civil War, the government expanded on this model of domiciliary care and created the National Home for Disabled Volunteer Soldiers. Over the next 40 years, the different branches of the National Home system provided room, board, and medical assistance to more than 100,000 indigent or infirm Union Veterans.
U.S. participation in the First World War produced a profound shift in public policy away from the reliance on long-term institutional care for Veterans in need. During the war, the federal government embraced a new model of Veteran welfare centered around short-term hospitalization in professional medical facilities, supplemented with physical and vocational rehabilitation to help those with disabilities return to the work force.
The revised War Risk Insurance Act passed by Congress in 1917 committed the nation to delivering “governmental medical, surgical, and hospital services” to disabled servicemembers. At first, the War Department assumed responsibility for tending to the sick and wounded. Over the course of the war, the Army expanded its convalescent capabilities twelve-fold, establishing over 100 hospitals and acquiring enough beds to accommodate 123,000 patients. The U.S. Public Health Service (PHS) supported this effort. Founded in 1798 within the Treasury Department, PHS carried out a variety of missions to promote the health and welfare of the nation. It conducted medical research, enforced quarantines to stem the outbreak of disease, and examined immigrants at their ports of entry, among other tasks. The agency also operated some 20 marine hospitals for the benefit of merchant seaman and Coast Guard personnel. When the United States entered the war in 1917, President Woodrow Wilson ordered all PHS hospital facilities to admit patients from the Army and Navy in locales lacking a military hospital. In addition, medical officers from the PHS were detailed to the military upon request of the service secretaries.
The War Department’s plans for treating the sick and wounded were based on the premise that patients would receive up to six months of care in a military hospital, after which they would be restored to health and returned to the ranks or discharged if no longer fit for service. What government and military officials did not count on was that some servicemembers would require longer periods of hospitalization. Furthermore, many of those discharged also needed medical care. This was particularly true for tuberculosis sufferers, who numbered over 20,000. Once the November 1918 armistice brought the Great War to a close, the Army began to dismantle its hospital system, reducing the number of beds available in general hospitals to 40,000 by May 1919 and 3,000 by October 1920.

At this juncture, the Public Health Service stepped in to fill the breach, providing hospital beds and medical care to Veterans with service-connected conditions. Besides treating the sick and injured, PHS doctors also carried out examinations of Veterans to determine their eligibility for disability compensation and vocational rehabilitation. To meet the increased demand for hospitalization services, the agency leased or purchased facilities the Army and Navy no longer wanted as well as other properties that could be used for medical purposes. In the spring of 1919, Congress also approved the largest federal hospital construction program in U.S. history to date, appropriating more than $9 million for the building of new hospitals and the improvement of existing ones. By June 1920, the PHS reported that it was operating an additional 28 hospitals of three different types: general medical, tuberculosis, and neuropsychiatric. Agency officials asserted, however, that its medical resources still fell far short of what it needed to handle the expected surge in the number of Veterans seeking treatment over the next few years. Congress heeded the PHS’s warnings and appropriated a staggering $35.6 million for more hospital construction in two landmark acts passed in 1921 and 1922.
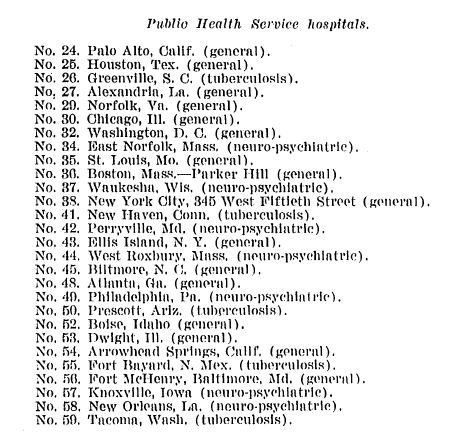
By the time the second of these bills became law, Public Health Service’s stewardship of the expanding Veteran hospital network had come to an end. After the war, Veterans and their advocates in organizations like the American Legion had grown increasingly unhappy with the way the federal government managed their benefits and services. Programs for World War I Veterans were spread across three separate agencies—PHS for hospital care, the Bureau of War Risk Insurance for compensation and insurance, and the Federal Board of Vocational Education for rehabilitation and job training. The American Legion led the way in lobbying Congress to consolidate of all of these programs in a single office. The demands for reform produced the desired results. In 1921, Congress created the Veterans Bureau, an independent federal agency with expansive authority, a huge workforce, broad responsibilities, and a budget that was one the largest in the government. The following year, PHS transferred all Veterans hospitals under its control, which by then numbered 57, along with much of its medical staff to the new bureau.
Under the Veterans Bureau, the nascent Veteran health care system continued to grow. In the 1920s, the bureau established a medical research program, diagnostic centers, top-notch laboratories, and a medical bulletin. Veterans could receive in-patient treatment at one of the state-of-the-art hospitals funded by Congress or out-patient care at dozens of different clinic locations. A further consolidation of Veterans medical facilities took place in 1930 when the Veterans Administration replaced the Veterans Bureau and took charge of all National Home properties. By the eve of World War II, the ad hoc medical program overseen by the Public Health Service for Great War Veterans had evolved into a full-service system that ministered to the health and hospital needs of all Veterans.
By Darlene Richardson, Historian, Veterans Health Administration (Retired), and Jeffrey Seiken, Ph.D., Historian, Veterans Benefits Administration
Share this story
Related Stories
History of VA in 100 Objects
In the waning days of World War I, French sailors from three visiting allied warships marched through New York in a Liberty Loan Parade. The timing was unfortunate as the second wave of the influenza pandemic was spreading in the U.S. By January, 25 of French sailors died from the virus.
These men were later buried at the Cypress Hills National Cemetery and later a 12-foot granite cross monument, the French Cross, was dedicated in 1920 on Armistice Day. This event later influenced changes to burial laws that opened up availability of allied service members and U.S. citizens who served in foreign armies in the war against Germany and Austrian empires.
History of VA in 100 Objects
Basketball is one of the most popular sports in the nation. However, for paraplegic Veterans after World War II it was impossible with the current equipment and wheelchairs at the time. While VA offered these Veterans a healthy dose of physical and occupational therapy as well as vocational training, patients craved something more. They wanted to return to the sports, like basketball, that they had grown up playing. Their wheelchairs, which were incredibly bulky and commonly weighed over 100 pounds limited play.
However, the revolutionary wheelchair design created in the late 1930s solved that problem. Their chairs featured lightweight aircraft tubing, rear wheels that were easy to propel, and front casters for pivoting. Weighing in at around 45 pounds, the sleek wheelchairs were ideal for sports, especially basketball with its smooth and flat playing surface. The mobility of paraplegic Veterans drastically increased as they mastered the use of the chair, and they soon began to roll themselves into VA hospital gyms to shoot baskets and play pickup games.
History of VA in 100 Objects
After World War I, claims for disability from discharged soldiers poured into the offices of the Bureau of War Risk Insurance, the federal agency responsible for evaluating them. By mid-1921, the bureau had awarded some amount of compensation to 337,000 Veterans. But another 258,000 had been denied benefits. Some of the men turned away were suffering from tuberculosis or neuropsychiatric disorders. These Veterans were often rebuffed not because bureau officials doubted the validity or seriousness of their ailments, but for a different reason: they could not prove their conditions were service connected.
Due to the delayed nature of the diseases, which could appear after service was completed, Massachusetts Senator David Walsh and VSOs pursued legislation to assist Veterans with their claims. Eventually this led to the first presumptive conditions for Veteran benefits.